Stereotactic radiation therapy for recurrent nasopharyngeal carcinoma
Introduction
Nasopharyngeal carcinoma is particularly prevalent in East Asia and Southeast Asia. Its incidence has declined gradually but steadily, and its mortality has been reduced substantially. These improvements are most likely the result of changes in lifestyle and environment, enhanced understanding of the pathogenesis and risk factors, population screening, and advancement in imaging techniques. Radiation therapy is the mainstay treatment for nasopharyngeal carcinoma, as it is highly sensitive to radiation. With the progression of induction, concurrent, and adjuvant chemotherapy with radiation therapy to treat nasopharyngeal carcinoma, patient survival has improved and toxicities have been reduced (1).However, approximately 10% of patients develop recurrent disease (2), and the median recurrence period is approximately 30 months, with 85% of local recurrences being detected within 5 years (3). Surgery, reirradiation, and systemic therapy can be used to treat local recurrent nasopharyngeal carcinoma. Retrospective studies have indicated that the salvage rates for surgery and reirradiation are similar (4). Various confounding factors, such as lower disease volume, earlier r-T stage (recurrent tumor stage), performance status, and medical comorbidities, limit resectability for recurrent nasopharyngeal carcinoma (5).
Reirradiation is the most common approach for recurrent nasopharyngeal carcinoma. Various radiobiological factors, as well as the dose tolerance of organs at risk (OARs) (mucosa, carotid vessels, and neurological structures) should be carefully considered due to prior radiation dose exposure in primary treatment.
Salvage surgery to recurrent nasopharyngeal carcinoma
Aggressive salvage treatment should be considered as much as possible, as long-term survival is still possible for most patients. Local disease can be controlled with surgery; however, there is a high risk of complications after treatment (6-8). Na’ara et al. conducted a meta-analysis for the outcome of patients undergoing salvage surgery for recurrent nasopharyngeal carcinoma (9). The 5-year overall survival and local recurrence-free survival rates were 51.2% and 63.4%, respectively. Patients who received surgery and adjuvant radiation therapy had a 5-year overall survival rate of 63% compared with a significantly lower rate of 39% in patients who received surgery alone. Liu et al. reported a multicenter, randomized, controlled phase 3 trial comparing endoscopic surgery with intensity-modulated radiotherapy (IMRT) in resectable locally recurrent nasopharyngeal carcinoma (10). The eligible criteria were recurrent tumor confined in one or more of the following resectable areas: the nasopharyngeal cavity (rT1), the postnaris or nasal septum (rT2a), the superficial parapharyngeal space (rT2b), or the base wall of the sphenoid sinus (rT3). Other eligibility criteria were as follows: being free of regional lymph node recurrence and at least a 12-month disease-free interval. The 3-year overall survival was 85.8% in the surgery group and 68% in the IMRT group; 5% of the patients who underwent surgery and 20% who underwent IMRT died as a result of late toxic effects. Salvage surgery, on the other hand, tends to yield betters result in the low-recurrence stage. Patients with locally recurrent nasopharyngeal carcinoma may undergo either radiotherapy or surgery, but the salvage endoscopic surgery approach is still relatively new, with limited information and experience regarding it outcomes (11). Furthermore, surgery to the nasopharynx is challenging due to the risk of damaging various neurovascular structures, including the dura mater (12). Thus, reirradiation remains the most common treatment for recurrent nasopharyngeal carcinoma.
Fractional radiation therapy to recurrent nasopharyngeal carcinoma
The conventional radiation therapy scheme is fractionated, which means that the treatment is delivered over several weeks, one day at a time. The cells within the tumor go through different phases of cell cycle, and after radiation exposure, cells die due to DNA damage. The poor DNA-repairing function allows the radiation to be more effective against the tumor, and the normal tissues are more capable of repairing damage if the dose is delivered in smaller daily treatments. The most reirradiation protocol to recurrent tumor volume was found to yield a 3- to 5-year local control rate of 44.3–85.8%, respectively (13,14). The reported 3- to 5-year survival rates for fractionation radiation therapy to recurrent nasopharyngeal carcinoma range from 27.5% to 63.8% (15,16). The reirradiation dose may be a key factor in salvage rates. For a planned radiation dose of ≤60 Gy, 3- to 5-year local control rates have been reported between 44.3% and 52% (14,17), while for a dose of >60 Gy,the 3- to 5-year local control rates reported range from 60.9% to 85.1% (15,18). Whereas, the 3- to 5-year overall survival rates ranged from 47.5% to 63.8% for a planned radiation dose of ≤60 Gy (16,17) and 27.5% to 51.5% for a planned radiation dose >60 Gy (15,19). However, severe complications during the second course of radiation therapy are not uncommon. Mucosa necrosis, carotid blowout, skull base osteonecrosis, temporal lobe necrosis, and other serious complications can occur after reirradiation for recurrent nasopharyngeal carcinoma (20-22). Because of the narrow therapeutic margin, a higher radiation dose may not result in a better survival, as fatal complications negate the benefit of higher tumor control rates (23). Although the tolerated dose of OARs in second radiation therapy has been proposed for partial recovery (24-26), all of these models are based on sparse clinical information with the details of dose distribution within the OARs being unknown. Therefore, the allowable tolerated dose for OARs in the second course of radiation therapy should always be guided by the “as low as reasonably practicable” (ALARA) principles to avoid critical complications (27). Therefore, similar consideration should be applied to the design of reirradiation volume, and the elective treatment (e.g., uninvolved regional nodal or sub clinical disease) is not recommended (28). The treatment targets for recurrent nasopharyngeal carcinoma usually consist of the recurrent gross tumor volume (rGTV) with a tight margin.
Stereotactic radiation therapy (SRT)
SRT developed from hypofractionated stereotactic radiosurgery (SRS). The cobalt-60 isotope, which is gamma knife, was first proposed as a source of radiation for SRS (29). By 1980, linear accelerators with artificial x-ray beam sources could also irradiate lesions from multiple angles to perform SRS, due to the modification of using special equipment packages. As technology progresses, numerous specially designed radiation therapy devices, such as Cyberknife, TomoTherapy (Accuray, Sunnyvale, CA, USA), or Novalis (BrainLab, Munich, Germany), are being developed for SRT with fractionated potential. All of these devices use computer-based stereo positioning guidance to ensure that the radiation rays are transmitted accurately to the treatment target SRS (30). However, SRT may still deliver a considerable dose to critical organs, and thus a treatment of choice for recurrent tumors still needs to be developed. The choice of treatment should have therapeutic benefits to the patient, both in terms of tumor control and complications. There is also risk in surgical intervention when the recurrent nasopharyngeal tumor is near the carotids, and the surgery only has one change to be treated in the operating room. However, with SRT, it is possible to optimize the treatment plan through iterative calculations on the computer until compromise is encountered, allowing recurrent tumors to be irradiated with a sufficient dose without affecting the carotid artery. SRT techniques may represent an ideal treatment modality for recurrent nasopharyngeal carcinoma in that they can escalate the radiation dose to rGTV with an as-low-as-possible dose to OARs, thus avoiding fatal complications.
SRT for recurrent nasopharyngeal carcinoma
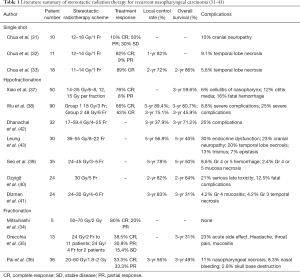
SRT is a highly precise treatment technique. As SRT can deliver a very specific radiation dose with a rapid dose fall-off, the dose to nearby OARs is kept as low as possible. To escalate the biologic effect of the treatment, treatments are normally hypofractionated with a high-fractionated dose (e.g., above 4 Gy per fraction at 3–5 times treatment). SRT can also be used to perform single or conventional fractions. The available reports for recurrent nasopharyngeal carcinoma using SRT technique are listed in Table 1. Chua et al. (31-33) used single-shot SRT with a 11–18 Gy single fraction treatment for recurrent nasopharyngeal carcinoma and reported a response rate of 60–91% (including complete and partial response). The reported local control rates were 82% for 1 year and 72% for 2 years. Furthermore, patients with rT1 disease also had a better outcome following single-shot radiation therapy compared with those with rT2 disease: the control rate was 77% (10 of 13) for rT1 disease and 40% (2 of 5) for rT2 disease (33).In single-shot SRT, the treatment volume may be a significant factor for treatment response. A large treatment volume may also induce severe complications with a high radiation dose. Sequelae with 10% cranial neuropathy and 5.6–10% temporal lobe necrosis have been reported in the literature (31-33). While a large single dose of radiation may overcome the tumor cell’s relative resistance to traditional fraction, a large treatment volume combined with a high radiation dose may not only restrict treatment response but also increase the risk of serious neurological complications. Single-shot SRT is suggested in patients with recurrent nasopharyngeal tumor at an early stage and with small tumor volume.
Full table
Conventional fractionation using the SRT techniques, instead of single-shot SRT, has also been attempted to treat recurrent nasopharyngeal carcinoma. Fractionated radiation based on radiobiologic principles should be more effective because of an improved therapeutic ratio, which enhances tumor control while reducing normal tissue damage. Typically, SRT aims the radiation dose to a recurrent nasopharyngeal tumor with a rapid fall-off, which can further reduce the impact of radiation on underlying normal tissue. There have been reports of fractional SRT being used to treat recurrent nasopharyngeal cancer (34-36). The reported treatment doses ranged from 20 to 70 Gy with fraction sizes ranging from 1.8 to 2 Gy. An 80% complete response rate with no severe complications was observed by Mitsuhashi et al. (34), Orecchia et al., and Pai et al., who reported response rates ranging from 66.6% to 69.3% and complete response rates ranging from 33.3% to 38.5% (35,36). In Orecchia et al.’s study, the 3-year local control rate was 56%, and the overall survival rate ranged from 31% to 49%. The incidence of acute side effects, including headache, throat pain, and mucositis, were 23% (35).Meanwhile, Pai et al. reported an 11% incidence of nasopharyngeal necrosis, 8.3% nasal bleeding, and 2.8% skull base destruction using fractionation SRT (36). Neither the risk of complication nor the treatment response was better under fractionated SRT as compared with to the single-shot modality. It may be that a single shot is more effective and capable of sterilizing malignant tumors while the precision of SRT technique is reduced by repeated daily treatment that increases the risk of radiation therapy–related complications.
Hypofractionated radiation therapy, in which the dose is divided into larger doses than conventional radiotherapy is, can be used instead of a single-shot large-dose radiosurgery, and treatments are given once a day or less often. Therefore, hypofractionated radiation therapy is given in a shorter period (i.e., over several days) than is conventional radiation therapy. To minimize complications, this treatment scheme should have effective malignant cell sterilizing power close to that of single-shot and normal tissue damage-repair ability. Most study series examining hypofractionated SRT for recurrent nasopharyngeal carcinoma tended to have more cases than did single-shot and conventional fraction studies. The treatment radiation dose ranged from 17 to 59.4 Gy with 3–25 fractions (37-41). Except for a few series that used around 2.5 Gy (42,43), most series used 3–6 fractions with a fraction size of 4.25–15 Gy (37-41). The response rates ranged from 66.6% to 90% with the best complete response rate reported being 76% (37). The local control rates were similarly high, with rates of 82%, 89%, and 78% being reported at 2-, 3-, and 5-year follow-up, respectively. The highest overall survival rates reported at 2-, 3-, and 5-year follow-up were 64%, 80%, and 50%, respectively. The 3-year local control rates for the studies using fraction sizes of around 2.5 Gy, which is similar to that of traditional radiation therapy, ranged from 37.9% to 56.8% (37-41). The 3- and 5-year overall survival rates were at least 71.2% and 40%, respectively in the hypofractionation SRT series (42,43). In regard to radiation complications, although the rate of severe complications may be as high as 25%, the fatal complications were 12.5% to 16% in all hypofractionated SRT series. Nonetheless, incidences of endocrine dysfunction, cranial nerve neuropathy, and temporal lobe necrosis of 30%, 23%, and 20%, respectively, were reported even with a smaller fraction dose of about 2.5 Gy (43). The treatment response, local control rate, and overall survival of hypofractionated SRT appear to be superior with an about equal complication rate compared with conventional fraction SRT.
According to the above results, hypofractionated SRT for recurrent nasopharyngeal carcinoma appears to be a reasonable treatment strategy. The treatment response is better than conventional radiation therapy due to the radiobiological effect of the large fraction dose with the radiation-induced complications being reduced due to the time gap between fractions for normal tissue repairing. Hypofractionated SRT also has the advantage of allowing patients to spend less time in the hospital for treatment, which is beneficial in large countries or remote areas where getting to the hospital is difficult. Radiation dose schemes reported in the literature vary widely, ranging from 14 to 55 Gy with fraction sizes from 4 to 15 Gy (Table 1). Recurrent nasopharyngeal cancer has various conditions with the goals of treatment being different in each case; thus, there is no standard radiation therapy protocol to follow. Furthermore, the constraints of the radiation therapy treatment plan for recurrent nasopharyngeal carcinoma are highly dependent on the results of initial radiation therapy. Therefore, SRT therapy planning and schemes should be based on the patient’s clinical condition, the accessibility of technology and treatment machines, the physician’s expertise, and relevant data from the literature.
SRT and salvage surgery are both local treatments. In a comparison of the results of surgery and SRT in recurrent nasopharyngeal carcinoma, surgery showed a lower fatal complication rate of 5% (10). However, the salvage surgery approach is still relatively new, with limited information and experience, and it is challenging due to the risk of damage to various neurovascular structures, including dura mater (11,12). SRT should be preferred for most recurrent nasopharyngeal carcinoma cases unless an experienced surgeon is available.
There are also limitations of SRT in recurrent nasopharyngeal carcinoma. First, there are technological requirements for SRT to ensure the desired quality for treatment. The requirements include imaging, motion management, treatment unit accuracy, and delicate quality assurance measures (44). Not all hospitals have the necessary equipment and technology to perform SRT, so this treatment is not widely available. The indications for SRT in the treatment of recurrent nasopharyngeal carcinoma are also limited. Due to the precision and accuracy requirements of SRT, the patient’s performance status should be good enough to remain stable during treatment for a sufficient period. Moreover, the treatment target volume is limited for SRT. The size of the lesion suitable for SRT should not exceed 3.5 cm in diameter. The treatment dose should also be reduced as the treatment volume increases. Nasopharyngeal carcinoma tends towards lymphatic metastases. As SRT lacks radiation dose focusing, it cannot be used if the recurrent tumor is too large or accompanied by lymphatic spread. Although SRT is an option for the treatment of recurrent nasopharyngeal carcinoma, the treatment decision should depend on the overall clinical condition of the patient.
Discussion
As nasopharyngeal carcinoma is highly sensitive to radiation, radiation therapy is the mainstay treatment modality. The survival of nasopharyngeal carcinoma patients has been improved with reduced toxicity of treatment due to the progression of induction, concurrent, and adjuvant chemotherapy with radiation therapy. However, 10% of patients still develop recurrent disease. The most common approach to recurrent nasopharyngeal carcinoma is reirradiation. Because of various radiobiological factors and the dose tolerance of OARs (e.g., mucosa, carotid vessels, and neurological structures), the prior radiation dose exposure in primary treatment should be carefully considered. The conventional radiation therapy scheme is fractionated, and the reirradiation dose may be a key factor in salvage rates. However, severe complications are not uncommon during the second course of radiation therapy, as the radiation dose to normal tissue that is tolerable is difficult to limit with the conventional radiation therapy technique. SRT can deliver radiation to a specific target with a rapid dose fall-off to surrounding normal tissue. It may represent an ideal treatment modality for recurrent nasopharyngeal carcinoma, as it can optimize the radiation dose to rGTV with an as-low-as-possible dose to OARs, which otherwise may be susceptible to fatal complications under larger doses.
SRT can be performed with conventional fractionation, hypofractionation, or single shot methods. While a large single dose of radiation may overcome the tumor cell’s relative resistance to traditional fraction, a large treatment volume combined with a high radiation dose may not only restrict treatment response but also increase the risk of serious neurological complications. Single-shot SRT is suggested for recurrent nasopharyngeal tumor in patients at the early stage of the disease and who have a small tumor volume. In contrast to use of the single-shot approach, SRT with conventional fractionated does not reduce the risk of complications and does not yield superior response rate. This may be due to the superior sterilizing effect on malignant tumors of the single-shot approach, and the tendency of the precision of SRT to be reduced by repeated daily treatment which may also increase the risk of radiation therapy-related complications. In comparison with conventional radiotherapy, hypofractionated radiation therapy divides the treatment dose into a larger dose per fraction. The treatment is given in a shorter period and can sterilize malignant cells with similar efficacy to that of the single-shot approach, while inflicting manageable tissue damage with minimal complications. The treatment response, local control rate, and overall survival seem to be better with an acceptable complication rate as compared to single-shot and conventional fractionated SRT.
On the other hand, SRT requires high technical standards to ensure the precision of the treatment, and the treatment target volume is often limited. This treatment may not be for patients who are unable to remain still during irradiation. SRT is not recommended for cases of recurrent nasopharyngeal carcinoma with lymphatic spreading due to its large target volume. Ng et al. have proposed international recommendations for reirradiation of locally recurrent nasopharyngeal carcinoma (45). The surgical resection is the preferred option, but the requisite expertise should be available, and a clear margin is likely to be achievable. SRT with its characteristic dose conformity and precision setup is a potentially advantageous modality with effective tumor control for low volume recurrent nasopharyngeal carcinoma. However, the possibility of serious toxicities (including damage to the central nervous system, fatal carotid blowout syndrome, or massive hemorrhage from mucosal/tissue necrosis) should be carefully considered. SRT for recurrent nasopharyngeal tumor near critical organs, especially neural tissue or carotid vessel, should be applied with care (40,43). Dose constraints of OARs for recurrent nasopharyngeal carcinoma are suggested for treatment with fractionation IMRT (45). Although published standards exist for SRT, the radiation doses of OARs in SRT could be converted to a biologically equivalent dose and summed with the doses of the primary radiation therapy for evaluation. The guiding principle should always be ALARA. Amid all the uncertainties and difficulties, the high-consensus recommendation of a safe, cumulative dose of reirradiation for recurrent nasopharyngeal carcinoma is ≤130% which can be fully tolerated by the brainstem, spinal cord, optic nerve, and temporal lobe; meanwhile, there is a moderate consensus of a ≤130% dose for the optic chiasm and a low-consensus dose of ≤125 Gy for the carotid artery. However, less stringent dose constraints, with the understanding and consent from the patient that less critical OARs may be damaged, can be considered to minimize salvage failure should the dose for the recurrent tumor be found inadequate.
Conclusions
In conclusion, for limited-volume local recurrent nasopharyngeal carcinoma, SRT is a valid option. However, compared with SRT, surgery or fractionation radiation therapy may be less likely to result in catastrophic toxicity. Patients should be counseled carefully before undergoing SRT, particularly if the target is close to a vital organ and could result in severe side effects. Although SRT has certain therapeutic advantages for recurrent nasopharyngeal carcinoma, conventional fractionation radiation therapy may still be the appropriate approach for reirradiation. The treatment decision should depend on the general condition and clinical disease status of the recurrent nasopharyngeal carcinoma patient.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the guest editors (Wai-Tong Ng, Shao Hui Huang, Hai-Qiang Mai) for the series “Precision Radiotherapy in Nasopharyngeal Carcinoma” published in Annals of Nasopharynx Cancer. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/anpc-21-2). The series “Precision Radiotherapy in Nasopharyngeal Carcinoma” was commissioned by the editorial office without any funding or sponsorship. YJH and FMF serve as the unpaid editorial board member of Annals of Nasopharynx Cancer from Apr 2018 to Dec 2021. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chen YP, Chan ATC, Le QT, et al. Nasopharyngeal carcinoma. Lancet 2019;394:64-80. [Crossref] [PubMed]
- Mao YP, Tang LL, Chen L, et al. Prognostic factors and failure patterns in non-metastatic nasopharyngeal carcinoma after intensity-modulated radiotherapy. Chin J Cancer 2016;35:103. [Crossref] [PubMed]
- Au KH, Ngan RKC, Ng AWY, et al. Treatment outcomes of nasopharyngeal carcinoma in modern era after intensity modulated radiotherapy (IMRT) in Hong Kong: A report of 3328 patients (HKNPCSG 1301 study). Oral Oncol 2018;77:16-21. [Crossref] [PubMed]
- Lee AW, Fee WE Jr, Ng WT, et al. Nasopharyngeal carcinoma: salvage of local recurrence. Oral Oncol 2012;48:768-74. [Crossref] [PubMed]
- Chan JYW, Wong STS, Wei WI. Surgical salvage of recurrent T3 nasopharyngeal carcinoma: Prognostic significance of clivus, maxillary, temporal and sphenoid bone invasion. Oral Oncol 2019;91:85-91. [Crossref] [PubMed]
- Chua DT, Sham JS, Kwong DL, et al. Locally recurrent nasopharyngeal carcinoma: treatment results for patients with computed tomography assessment. Int J Radiat Oncol Biol Phys 1998;41:379-86. [Crossref] [PubMed]
- Teo PM, Kwan WH, Chan AT, et al. How successful is high-dose (> or = 60 Gy) reirradiation using mainly external beams in salvaging local failures of nasopharyngeal carcinoma? Int J Radiat Oncol Biol Phys 1998;40:897-913. [Crossref] [PubMed]
- Yu KH, Leung SF, Tung SY, et al. Survival outcome of patients with nasopharyngeal carcinoma with first local failure: a study by the Hong Kong Nasopharyngeal Carcinoma Study Group. Head Neck 2005;27:397-405. [Crossref] [PubMed]
- Na'ara S, Amit M, Billan S, et al. Outcome of patients undergoing salvage surgery for recurrent nasopharyngeal carcinoma: a meta-analysis. Ann Surg Oncol 2014;21:3056-62. [Crossref] [PubMed]
- Liu YP, Wen YH, Tang J, et al. Endoscopic surgery compared with intensity-modulated radiotherapy in resectable locally recurrent nasopharyngeal carcinoma: a multicentre, open-label, randomised, controlled, phase 3 trial. Lancet Oncol 2021;22:381-90. [Crossref] [PubMed]
- Thamboo A, Patel VS, Hwang PH. 5-year outcomes of salvage endoscopic nasopharyngectomy for recurrent nasopharyngeal carcinoma. J Otolaryngol Head Neck Surg 2021;50:12. [Crossref] [PubMed]
- Li W, Lu H, Wang H, et al. Salvage Endoscopic Nasopharyngectomy in Recurrent Nasopharyngeal Carcinoma: Prognostic Factors and Treatment Outcomes. Am J Rhinol Allergy 2021;35:458-66. [Crossref] [PubMed]
- Han F, Zhao C, Huang SM, et al. Long-term outcomes and prognostic factors of re-irradiation for locally recurrent nasopharyngeal carcinoma using intensity-modulated radiotherapy. Clin Oncol (R Coll Radiol) 2012;24:569-76. [Crossref] [PubMed]
- Koutcher L, Lee N, Zelefsky M, et al. Reirradiation of locally recurrent nasopharynx cancer with external beam radiotherapy with or without brachytherapy. Int J Radiat Oncol Biol Phys 2010;76:130-7. [Crossref] [PubMed]
- Tian YM, Huang WZ, Yuan X, et al. The challenge in treating locally recurrent T3-4 nasopharyngeal carcinoma: the survival benefit and severe late toxicities of re-irradiation with intensity-modulated radiotherapy. Oncotarget 2017;8:43450-7. [Crossref] [PubMed]
- Ng WT, Ngan RKC, Kwong DLW, et al. Prospective, Multicenter, Phase 2 Trial of Induction Chemotherapy Followed by Bio-Chemoradiotherapy for Locally Advanced Recurrent Nasopharyngeal Carcinoma. Int J Radiat Oncol Biol Phys 2018;100:630-8. [Crossref] [PubMed]
- Chan OS, Sze HC, Lee MC, et al. Reirradiation with intensity-modulated radiotherapy for locally recurrent T3 to T4 nasopharyngeal carcinoma. Head Neck 2017;39:533-40. [Crossref] [PubMed]
- Kong F, Zhou J, Du C, et al. Long-term survival and late complications of intensity-modulated radiotherapy for recurrent nasopharyngeal carcinoma. BMC Cancer 2018;18:1139. [Crossref] [PubMed]
- Kong L, Wang L, Shen C, et al. Salvage Intensity-Modulated Radiation Therapy (IMRT) for Locally Recurrent Nasopharyngeal Cancer after Definitive IMRT: A Novel Scenario of the Modern Era. Sci Rep 2016;6:32883. [Crossref] [PubMed]
- Dong F, Li Q, Wu J, et al. Carotid blowout syndrome after nasopharyngeal carcinoma radiotherapy: successful treatment by internal carotid artery occlusion after stent implantation failure. Springerplus 2016;5:1553. [Crossref] [PubMed]
- Ng WF, Fung KH, Sham JS. Tension pneumocephalus--a rare complication of radiotherapy in nasopharyngeal carcinoma. Pathology 1995;27:204-8. [Crossref] [PubMed]
- Ye J, Rong X, Xiang Y, et al. A study of radiation-induced cerebral vascular injury in nasopharyngeal carcinoma patients with radiation-induced temporal lobe necrosis. PLoS One 2012;7:e42890 [Crossref] [PubMed]
- Xu T, Tang J, Gu M, et al. Recurrent nasopharyngeal carcinoma: a clinical dilemma and challenge. Curr Oncol 2013;20:e406-19. [Crossref] [PubMed]
- Lee AW, Foo W, Law SC, et al. Total biological effect on late reactive tissues following reirradiation for recurrent nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys 2000;46:865-72. [Crossref] [PubMed]
- Jones B, Hopewell JW. Alternative models for estimating the radiotherapy retreatment dose for the spinal cord. Int J Radiat Biol 2014;90:731-41. [Crossref] [PubMed]
- Jones B, Grant W. Retreatment of central nervous system tumours. Clin Oncol (R Coll Radiol) 2014;26:407-18. [Crossref] [PubMed]
- Lee AWM, Ng WT, Chan JYW, et al. Management of locally recurrent nasopharyngeal carcinoma. Cancer Treat Rev 2019;79:101890 [Crossref] [PubMed]
- Margalit DN, Wong SJ. Reirradiation for Head and Neck Cancer: The Who and the How. Int J Radiat Oncol Biol Phys 2018;100:618-20. [Crossref] [PubMed]
- Leksell L. The stereotaxic method and radiosurgery of the brain. Acta Chir Scand 1951;102:316-9. [PubMed]
- Adler JR Jr, Chang SD, Murphy MJ, et al. The Cyberknife: a frameless robotic system for radiosurgery. Stereotact Funct Neurosurg 1997;69:124-8. [Crossref] [PubMed]
- Chua DT, Sham JS, Hung KN, et al. Stereotactic radiosurgery as a salvage treatment for locally persistent and recurrent nasopharyngeal carcinoma. Head Neck 1999;21:620-6. [Crossref] [PubMed]
- Chua DT, Sham JS, Hung KN, et al. Salvage treatment for persistent and recurrent T1-2 nasopharyngeal carcinoma by stereotactic radiosurgery. Head Neck 2001;23:791-8. [Crossref] [PubMed]
- Chua DT, Sham JS, Kwong PW, et al. Linear accelerator-based stereotactic radiosurgery for limited, locally persistent, and recurrent nasopharyngeal carcinoma: efficacy and complications. Int J Radiat Oncol Biol Phys 2003;56:177-83. [Crossref] [PubMed]
- Mitsuhashi N, Sakurai H, Katano S, et al. Stereotactic radiotherapy for locally recurrent nasopharyngeal carcinoma. Laryngoscope 1999;109:805-9. [Crossref] [PubMed]
- Orecchia R, Redda MG, Ragona R, et al. Results of hypofractionated stereotactic re-irradiation on 13 locally recurrent nasopharyngeal carcinomas. Radiother Oncol 1999;53:23-8. [Crossref] [PubMed]
- Pai PC, Chuang CC, Wei KC, et al. Stereotactic radiosurgery for locally recurrent nasopharyngeal carcinoma. Head Neck 2002;24:748-53. [Crossref] [PubMed]
- Xiao J, Xu G, Miao Y. Fractionated stereotactic radiosurgery for 50 patients with recurrent or residual nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys 2001;51:164-70. [Crossref] [PubMed]
- Wu SX, Chua DT, Deng ML, et al. Outcome of fractionated stereotactic radiotherapy for 90 patients with locally persistent and recurrent nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys 2007;69:761-9. [Crossref] [PubMed]
- Seo Y, Yoo H, Yoo S, et al. Robotic system-based fractionated stereotactic radiotherapy in locally recurrent nasopharyngeal carcinoma. Radiother Oncol 2009;93:570-4. [Crossref] [PubMed]
- Ozyigit G, Cengiz M, Yazici G, et al. A retrospective comparison of robotic stereotactic body radiotherapy and three-dimensional conformal radiotherapy for the reirradiation of locally recurrent nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys 2011;81:e263-8. [Crossref] [PubMed]
- Dizman A, Coskun-Breuneval M, Altinisik-Inan G, et al. Reirradiation with robotic stereotactic body radiotherapy for recurrent nasopharyngeal carcinoma. Asian Pac J Cancer Prev 2014;15:3561-6. [Crossref] [PubMed]
- Dhanachai M, Kraiphibul P, Dangprasert S, et al. Fractionated stereotactic radiotherapy in residual or recurrent nasopharyngeal carcinoma. Acta Oncol 2007;46:828-33. [Crossref] [PubMed]
- Leung TW, Wong VY, Tung SY. Stereotactic radiotherapy for locally recurrent nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys 2009;75:734-41. [Crossref] [PubMed]
- Schmitt D, Blanck O, Gauer T, et al. Technological quality requirements for stereotactic radiotherapy: Expert review group consensus from the DGMP Working Group for Physics and Technology in Stereotactic Radiotherapy. Strahlenther Onkol 2020;196:421-43. [Crossref] [PubMed]
- Ng WT, Soong YL, Chan Ahn Y, et al. International Recommendations on Re-irradiation by Intensity-modulated Radiotherapy for Locally Recurrent Nasopharyngeal Carcinoma. Int J Radiat Oncol Biol Phys 2021; [Crossref] [PubMed]
Cite this article as: Huang YJ, Fang FM, Chen HC, Hsu HC. Stereotactic radiation therapy for recurrent nasopharyngeal carcinoma. Ann Nasopharynx Cancer 2021;5:5.